Description
Gynecomastia (enlargement of the male breast, puffy male nipples) is surprisingly common. It frequently begins during puberty but may also occur later. The cause of gynecomastia is unknown in most patients, though it has been linked to hormonal imbalance, excessive body weight, and certain drugs, such as anabolic steroids. Many teens and adults with enlarged breasts complain of self-consciousness and conceal the breasts with baggy clothing or multiple T-shirts. Most feel uncomfortable taking off their shirts in public.
Gynecomastia may include one or more of the following:
- Enlargement of the entire breast (due to excessive fat).
- Lumps or masses beneath the nipples (due to excessive fibroglandular breast tissues).
- Puffy or enlarged nipple-areolae (due to pressure from the underlying prominent tissues). The areola is the pigmented skin around the nipple.
Male Breast Reduction Before and After Photos


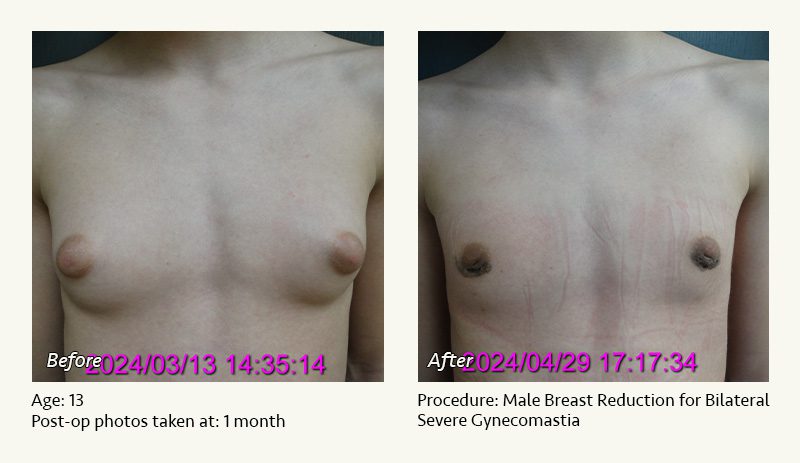
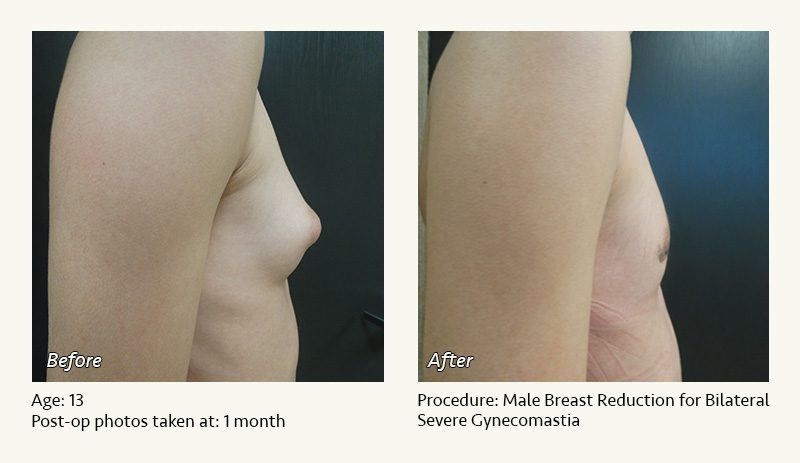
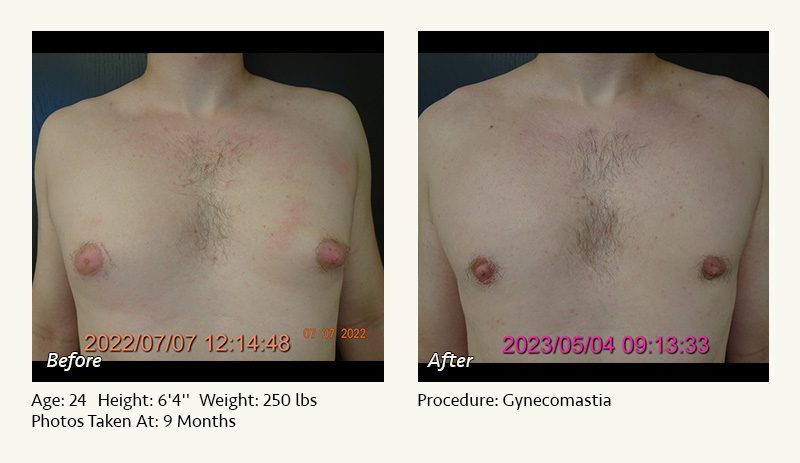

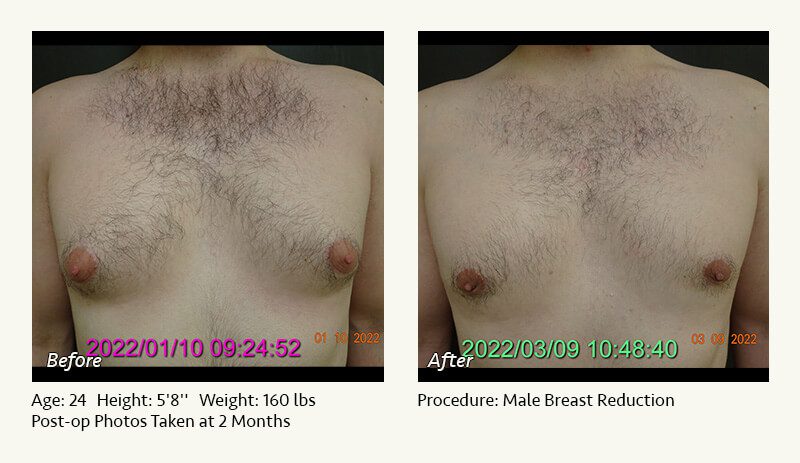







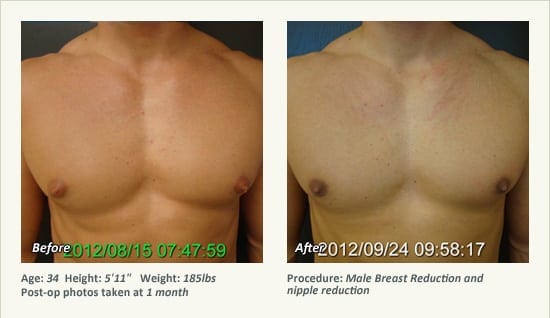









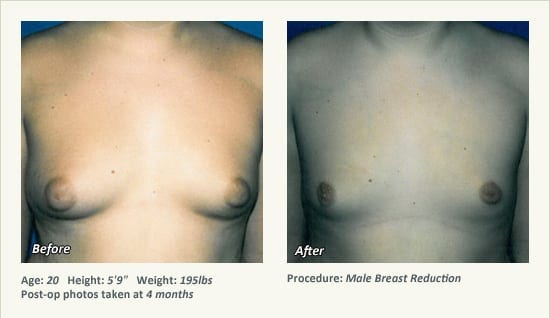
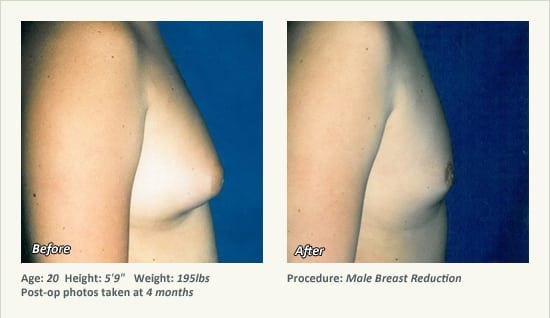

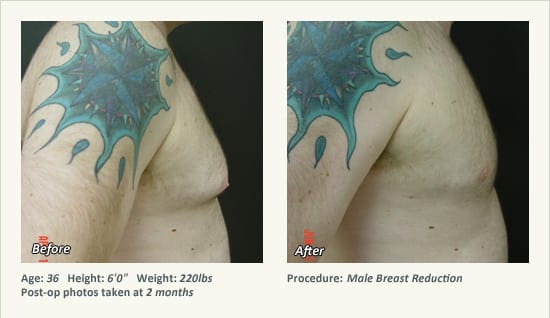


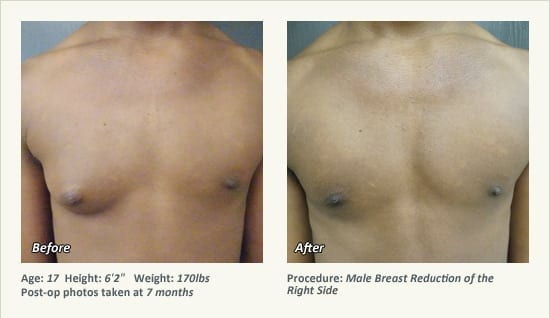

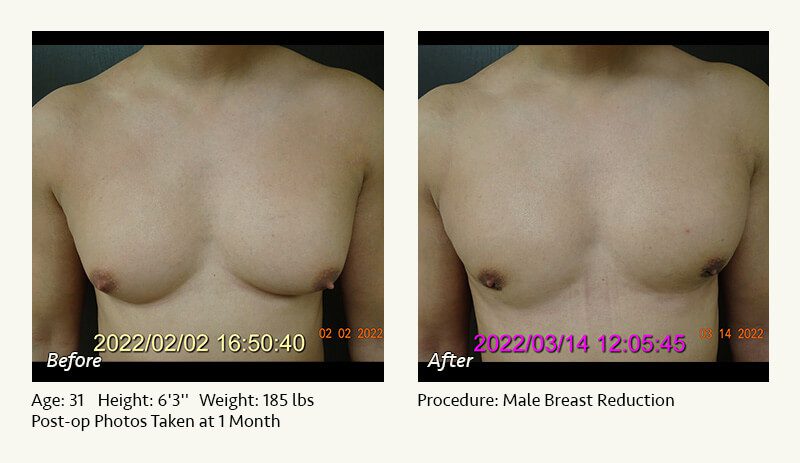


Male breast reduction (gynecomastia) is a surgical procedure performed to reduce the size of the breasts and/or the prominence of the nipple-areolae. In most patients, our Plano, Texas plastic surgeon, Dr. Friedman recommends liposuction of the breasts, which is performed through a single incision that is less than a quarter-inch in length. In men with prominent areolae or lumps beneath the areolae, he will also remove the excessive tissues through a short (less-than-an-inch) incision along the lower border of the areola.
Dr. Friedman attempts to minimize scarring by avoiding external stitches and making smaller incisions than those used by many surgeons. He generally blends the boundary of tissue removal through liposuction, minimizing the risk of a demarcation between the operated and unoperated areas of the chest.
In men who have isolated enlargement of the nipples (rather than puffiness or enlargement of the areolae), Dr. Friedman may perform nipple reduction under local anesthesia.
Dr. Friedman performs male breast reduction for gynecomastia under general anesthesia on an outpatient basis. The procedure is performed in his AAAASF-accredited surgical facility, the West Plano Plastic Surgery Center, which is located on the campus of Texas Health Presbyterian Hospital of Plano. He strictly uses physicians—not nurses or technicians—to administer your anesthesia.
Pain medication is necessary for about a week following surgery. Most patients return to light activities within 3 to 5 days, depending on the areas treated. A compression garment must be worn over the surgical sites continuously for one month and intermittently for a second month to maximize the surgical result.
When you visit our Plano, Texas office, Dr. Friedman will discuss your specific concerns. He will give you a realistic idea of what you can expect from surgery. We will also show you a variety of before and after photos of male breast reductions performed by Dr. Friedman. If you wish to speak to other patients who have undergone these procedures, we will be happy to provide phone numbers.
Watch Video: Dr. Friedman explains liposuction.
Q & A: Male Breast Reduction
-
What causes male breast reduction
Most cases of male breast enlargement are of unknown cause. Certain drugs (anabolic steroids, marijuana, spironolactone), hormonal conditions (excessive estrogen, deficient testosterone), and hereditary conditions may be associated with male breast reduction. Some men choose to see an endocrinologist for evaluation of potential causes, though the work-up is usually negative. Being overweight may also cause male breast enlargement.
-
What is the goal of surgery?
The goal of male breast reduction surgery is to allow you to go out in a light T-shirt (or go out to the pool without a shirt) without feeling self-conscious about the appearance of your chest. This requires reduction of excessive breast tissue through small, carefully placed incisions. Ideally, your chest should not look “operated,” as this may detract from the surgical results.
-
Will I have scars on my chest?
Any surgery involves scars. However, Dr. Friedman makes an effort to use the smallest possible incisions. When he does liposuction of the breasts, he uses a single less-than-a-quarter inch incision. When he does direct tissue removal, he generally limits the incision to less than an inch along the lower part of the areola (unlike many surgeons who utilize an incision along the entire lower half of the areola.
-
What if I my breast size is normal but my nipples protrude?
This is simply another, more localized form of gynecomastia. Typically this is addressed through a small incision along the lower part of the areola. Removal of excessive tissue that pushes the nipple-areolae forward will reduce the prominence of the nipples.
-
Will there be much pain?
Many teens considering male breast reduction worry about postoperative pain. While all surgeries involve pain, male breast reduction is generally well tolerated. Pain is usually moderate for a few days and then becomes much milder. Dr. Friedman will prescribe pain medication, which is usually necessary for about 5 to 7 days after surgery.
Male Breast Reduction: Instructions
One week before surgery
- Do not take aspirin-containing products, as these may increase your risk of bleeding. Use extra-strength Tylenol for any headaches or other minor pains.
- Please notify Dr. Friedman’s staff if you become sick with a fever, significant cough, etc. If necessary, your surgery can be rescheduled to a time when you are feeling better.
- Do not smoke at all or use a nicotine patch for at least two weeks (and preferably 4 weeks) prior to surgery and 4 weeks after surgery. Smoking interferes with wound healing and increases your risk for anesthetic and surgical complications.
- Arrange to have a relative or friend drive you home after surgery and stay with you for the evening. You cannot drive yourself home.
The evening before surgery
- Do not eat or drink anything for at least 8 hours prior to your scheduled surgery time.
- Make some jello and/or soup for after surgery. Have some juice in your refrigerator.
- The anesthesiologist will contact you by phone to discuss your medical history and to answer any questions.
Day of surgery: before you leave home
- Remember not to eat, drink, or smoke. This includes no chewing gum, mints, etc.
- Make sure someone is available to drive you home. Put a pillow and blanket in the car.
- Wear loose, comfortable clothing. Avoid contact lenses. Please do not use any lotion or powder. LEAVE ALL VALUABLES AT HOME!
Day of surgery: at the facility before surgery
- Dr. Friedman will talk to you before surgery to answer any last-minute questions. He will mark your chest to help him accurately plan your surgery.
- You will meet the anesthesiologist and surgical nurses.
Day of surgery: at the facility after surgery
- You will be taken to the recovery area to wake up after surgery. Dr. Friedman will go to the waiting room to speak to your family/friends.
- Approximately 1 hour later, your family can visit you. Once you are feeling well enough, you may go home.
At home after surgery
- Have someone stay with you for the first night. You may be weak and drowsy.
- Take the antibiotics, pain medication (as needed), and anti-nausea medicine (if needed) that Dr. Friedman has prescribed for you.
- Sleep with your head elevated. Sleep on your back (not your stomach or side).
- Leave the compression vest on for 3 days. On the third day after surgery, you may temporarily remove the garment and the underlying foam padding and begin showering. Wash your garment and then put the foam and the garment back on. You may shower daily.
- It is common to experience temporary drainage from the incision sites, which may be blood-stained. If the drainage is bloody and persistent, contact Dr. Friedman.
- Take at least 10 deep breaths every hour. This will help keep your lungs expanded.
- Do not be a couch potato. To reduce the risk of blood clots in the legs, get up and walk any time you need to eat or use the bathroom. While you are in bed, repeatedly flex your ankles (moving your toes up and then down) and/or have your family massage your calves.
- If you experience a prolonged fever (oral temperature greater than 101), contact Dr. Friedman. Feel free to call our office or to page Dr. Friedman for any other problems or concerns.
Instructions for your first postoperative visit (about one week after surgery)
- Activity level
1 week after surgery: you may resume casual walking but must not engage in vigorous exercise that increases your blood pressure or heart rate. You may resume driving once you are off of your pain medication. Avoid freeways until you are comfortable with city driving.
4 weeks after surgery: you may gradually resume exercise activity. You should wear your compression garment while you are exercising. - Sleeping position
Please sleep on your back (flat or elevated) or part way over (pillow under your shoulder and hip). Do not sleep on your side until about 3 weeks after surgery. Unless otherwise instructed by Dr. Friedman, do not sleep on your stomach until about 8 weeks after surgery. - Incision care
After your butterfly tapes and/or surgical glue peel off (about 2 weeks after surgery), begin scar massage with Mederma twice daily. Mederma is available at our front desk or over-the-counter at your pharmacy. If you prefer, you may use Vitamin E or Aloe Vera. Continue scar massage for about 3 months. - Massage
You should begin massage to the chest one week after surgery. This will help smooth any irregularities and areas of firmness. You may apply lotion to your hand to massage and/or you may use a vibrating massager. If you would like, we will provide you the phone number of a licensed massage therapist. - Water exposure
You may begin light showers 3 days after surgery. You should avoid scrubbing your incisions. Avoid the pool, lake, and ocean for 4 weeks. - Medications
One week after surgery, you may resume use of any medications or supplements that you discontinued prior to surgery. However, for at least 3 weeks, you should avoid Motrin, aspirin, and any other product that may thin your blood. - Smoking
Do not smoke for at least one month (and preferably much longer) after surgery. Smoking may increase your risk of infection, lung problems following anesthesia, and wound healing problems. - Tanning
You may tan whenever you like. However, you should use a high-SPF sunscreen (30 or greater) over your incisions for at least 6 months. Premature tanning of the incisions may cause them to darken permanently. - Sex
Adult males may resume intercourse about 3 weeks after surgery. You may not bear weight on your chest for at least 6 weeks. - Compression garment
Wear the compression garment all day and all night (except for showers and massage) during the first month. You may gradually taper your use of the compression garment over the second month.
Please feel free to ask Dr. Friedman or his staff about any additional questions or concerns.